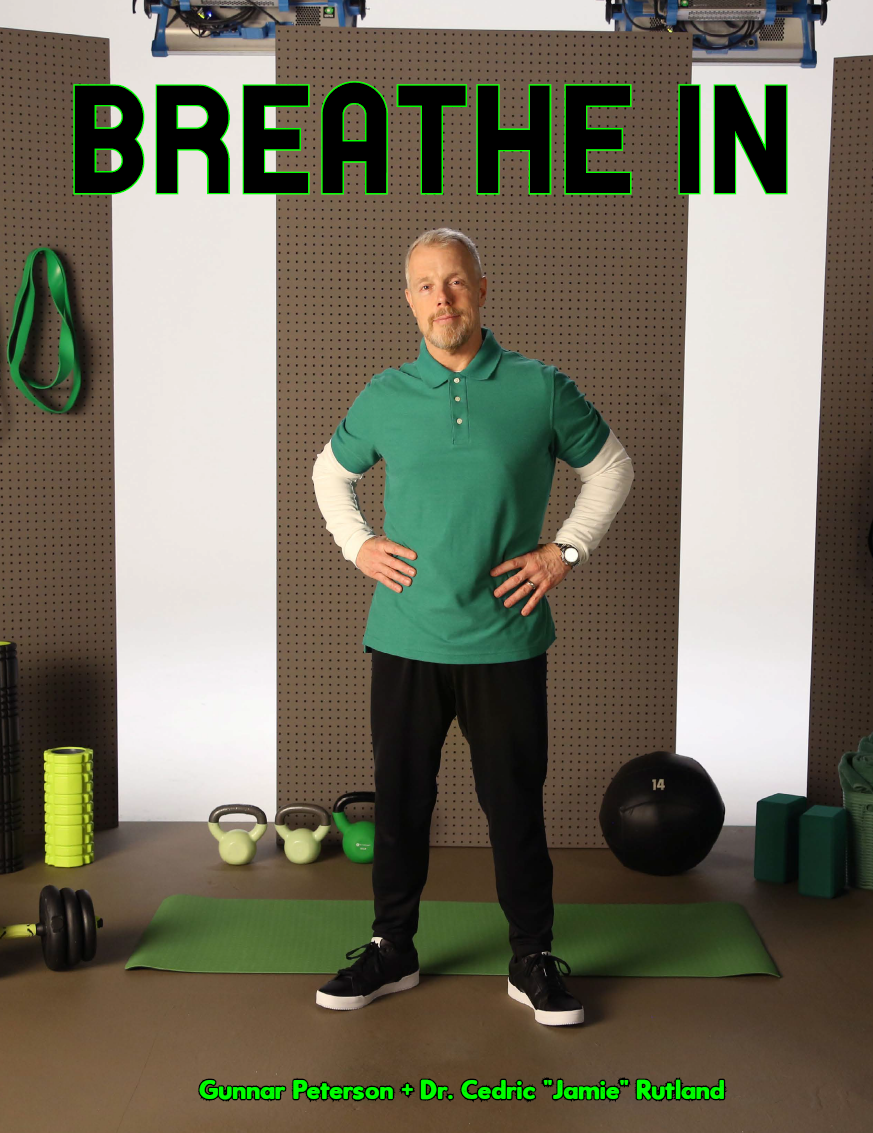
Gunnar shared how he is involved in LungZone and why this is important for those that are living with asthma. We wanted to take a step back and to take a look at asthma. It's important for us to take a step step back and look at what asthma is, how this condition affects the body and the areas that it targets specifically. Dr. Cedric "Jamie" Rutland, a pulmonologist, explains more about this to give us a better understanding about this and what are common triggers. It's impossible to think about asthma and its affects without asking about how COVID can also play into this condition and the importance of receiving the vaccine. He also shares his involvement in LungZone as well.
ATHLEISURE MAG: Before we delve into asthma, LungZone etc, I’d like to know about your background as you’re a fellow Big 10 alumni. Why did you want to work with those who have pulmonary issues?
DR. CEDRIC "JAMIE" RUTLAND: It's a great question. The way that I ended up at a Big 10 school, University of Iowa for medical school, was really that it just happened to be a top 10 medical school. So when I got accepted, I decided to go there. When you think about a Big 10 school in the Midwest in general, that area of the country is very well educated. All the students within that area of the country are so talented, and so good at being a student that I picked up a lot of different skills from others in the process. That experience truly allowed me to understand what pulmonary and critical care offered me, which was the opportunity to not only specialize in a certain field of medicine, but also experience other parts of medicine that I enjoy because when you're an ICU physician you see everything. I still like to help people with kidney problems, liver problems, and GI tract problems. ICU medicine also gave me the opportunity to communicate with families and patients in critical situations. It allowed me to explain things and teach, which is something that I really like to do, and I think without the help of a Big 10 school, like the University of Iowa, I wouldn't be where I am today.
AM: For our readers that may not be familiar with asthma, can you talk about what it is and the areas of the body that are affected?
DR. CJR: Let’s first talk about the lungs and how it's structured. The lung is essentially a bunch of pipes that lead to a bunch of balloons stacked on top of one another. When you take a deep breath, that air travels down your windpipe and further down into smaller little pipes called the bronchi and bronchioles. Those bronchioles lead to the balloons where oxygen is picked up by your blood and used to keep your body functioning properly.
Asthma is an inflammation of those pipes. More specifically, it's inflammation of the smooth muscle layer of the pipe, which leads to airway narrowing. That means people have trouble taking a deep breath in, and more specifically, even have trouble releasing a deep breath out. We want to calm that inflammation down so people can breathe easier and feel a little bit better.
AM: Are there various categories or groups as I’m sure that not all asthma is the same for those that have it.
DR. CJR: Yes, there are different categories and different treatments depending on the type of asthma you have. If a patient comes in and tells me they are short of breath, I quickly determine what type of inflammation may be present in their body. Those patients might need an inhaler. But, often times, it's not just a localized type of inflammation. It's often a systemic type of inflammation, something we call Type 2 inflammation. When you identify that more systemic type of inflammation, then there are certain treatment options that work to block that inflammation, like Dupixent® (dupilumab). In clinical trials, Dupixent improved lung function in as little as 2 weeks and helped reduce asthma attacks by up to 81% when compared to standard of care alone plus placebo. I should mention that people shouldn’t use Dupixent if they are allergic to it or its ingredients, and it can cause serious side effects, including allergic reactions and inflammation of your blood vessels. So, it’s important to talk to your doctor to see what type of inflammation you have and what type of treatment may be right for you.
AM: What are the symptoms of asthma and are there seasons where it can be more prone to happening?
DR. CJR: Common symptoms of asthma are shortness of breath, wheezing, and coughing. Those symptoms tend to happen as soon as you're exposed to irritants or anything that you are allergic to. If you go outside and its springtime and all that pollens around, and you start coughing or wheezing, that's going to be your trigger. If you are going outside during the wintertime, and you feel like your airways are narrowing or you start coughing then cold is your trigger. All these things can trigger your airways to become inflamed and that leads to airway narrowing, mucus production, shortness of breath and wheezing which are the classic symptoms of asthma.
AM: For those who are living with asthma, what do you suggest that they should be aware of when it comes to living a 360 life in terms of fitness whether they’re an enthusiast or an athlete?
DR. CJR: I think if you are an athlete or a fitness enthusiast who lives with asthma, then you have to understand your disease and listen to your body when it’s telling you that you don't have your disease under control. It's very important for people to be aware of their symptoms because the last thing you want is for that persistent inflammation to continue which could lead to a hospitalization, severe asthma attack and potentially death. If you're using an inhaler and you're still coughing or short of breath when you do things like going up a flight of stairs, you need to tell your physician – whether it's your primary care physician, your pulmonologist, or your allergist – that your medication isn’t working and see what else is out there.
AM: Can you tell me about what LungZone is, why you wanted to be involved in it and how you’re participating with this program.
DR. CJR: LungZone is a virtual community created by Sanofi and Regeneron to allow patients and their family members the opportunity to become educated about what asthma is, what inflammation is present in your lungs, and potentially how to treat that inflammation appropriately. The reason why I'm involved in LungZone is because as a doctor, it marries two things I'm in love with. One is immunology, which is the study of white blood cells and what they do in the body when there’s inflammation present. And the other thing is communication. I think it's very important for patients and their family members to understand what the body is going through. What I have found, is that people who understand what's going on in their body tend to tolerate their disease a little bit better, and they feel empowered by learning what's going on in their body and understanding how they can help control their disease. I think that that is something that is extremely important, and it's something I'm passionate about.
AM: How can our readers participate?
DR. CJR: Your readers can participate by going to JoinLungZone.com and taking my "Help Manage Your Asthma" class or take the other more dynamic classes from Gunnar Peterson and Kelley Green. I think what's good about these classes is that they truly help people understand what their body is going through, what they maybe need to ask their physician and other ways to strengthen their body and manage their systems.
AM: As we have all been navigating these past months due to COVID-19, can you share any information in terms of those who have actually battled COVID while being asthmatic or for those who have not had COVID but do have asthma how this may affect them?
DR. CJR: What's interesting about asthma is that there are different subcategories of asthma. Depending on the type of asthma, a person might deal with SARS-CoV-2 differently. Asthma leads to airway inflammation, and so does COVID-19. If asthma-related inflammation is uncontrolled, then COVID-related inflammation can be really problematic. If there's one thing that I've learned, it is making sure that a person's asthma symptoms and the inflammation are under control.
AM: Do those who are not asthmatic but have gotten COVID experience some of the issues that are similar to asthma?
DR. CJR: Yes, you can. Again, when you have that inflammation of lungs, whether it's caused by smoke, pollen, or COVID, the symptoms are going to be the same. I have had people who have never been diagnosed with asthma, that now have asthma due to this persistent inflammation in the post-COVID setting.
AM: For those that may not have received the vaccine for COVID and are asthmatic, what is your message to them to encourage them to get it?
DR. CJR: I love this question and I will tell you why. If you're a patient of mine, you're going to understand what asthma is and how it works. We talk a lot about targeting inflammation. The whole point of a vaccine is to calm down inflammation and not allow the immune system to overreact and cause more problems. It’s a lot easier for my patients to understand how and why a vaccine works. We also talked in the earlier questions about what complications COVID can cause when you have asthma, and that’s also what I discuss with my patients.
AM: You are a busy man without a doubt. You're the founder/ownder of West Coast Lung. Can you tell me more about this and why you wanted to launch your own office?
DR. CJR: When I was a young doctor, I understood that the most important people to be able to communicate with were not my colleagues, it was my patients. There was a particular incident when I was in the hospital, and a colleague of mine couldn't get a patient to open up. This lady looked exactly like my grandma. So, first thing I said to her was, "Good Afternoon Mama." And she just opened up to me. My colleague said to me, "How did you know to call her mama?" I said, "She's an African American female so she's mama, that's just who she is.” That's when I understood that I needed to make certain I knew how to communicate with patients. So, when I started West Coast Lung, I wanted to focus on messaging and education amongst patients and their family members, so they can understand what is going on with their bodies. I think it empowers people and allows them to more easily deal with what they have, and perhaps make some changes to their diet and exercise that helps them feel better in the long run.
AM: You’re also the VP of the Association for Healthcare Social Media. What is this organization and how are you involved?
DR. CJR: We knew that social media was going to be a place where people were going to get health information. We knew that 50% of people got their health information from social media, which was astonishing to us, but we also know with social media that you can post anything. We understand our role with messaging and how to combat misinformation, and that's what we are continuing to do. Our role in social media is continuing to evolve, and we partner with YouTube, Pinterest, and are always looking for other media partners to be able to express our message. We have physicians that discuss gastroenterology, fertility, and obstetrics. So, we really all understand the impact that social media has and as a company you want to be able to deal with it in a very positive way.
AM: You’re also the National Spokesperson of the Lung Association! What do you to bring awareness to lung health and how long have you been in this role?
DR. CJR: I've been involved with the American Lung Association for about four years. What I like about being a spokesperson, is that it gives you the opportunity to show that there are doctors who look like me on a national scale. I think that there's a lot of kids that look like me that may not know that they can be a doctor, or they can become a doctor, so I think that showcasing that was important to me. It also allows me to practice my craft around messaging and teaching on the national stage and explain things in a way that everybody can understand, which again I think is really important. Being in this position allows me to be that bridge between science and your everyday person.
AM: Going through your Instagram, it’s evident that you’re passionate about pulmonary issues and making it approachable through your videos. Why has this been important for you to share this kind of information socially?
DR. CJR: You have to be able to explain it in a way that people can understand. If you can't, you've done nothing. For example, with the COVID vaccines, within a year we went from having nothing to "go get the vaccine." We had a year to teach immunology.
I think in that moment I understood and said, "You know what, I am just going to teach how the body works." If people can understand that, maybe they can get to the conclusion of how a vaccine works. I teach why the vaccine may work, but I also teach about Onesimus, who was the African slave who brought the concept of vaccination to this country in the 1700s. I discuss why Onesimus had this belief in how smallpox should be treated and how that concept came from Africa to Boston during the smallpox pandemic. I want people to understand, and I use their language to make it happen.
AM: In addition to using your platform for health, it also looks like you enjoy having fun like your appearance on Game of Talents this past spring and sharing your wall of Js. How important is it to you that you have that work life balance as well as sharing that doctors come in many forms and can literally be a cool guy that you’d want in your friend group?
DR. CJR: I think it's important for people to be themselves and embrace who you are. I've done game shows with my friends. I'll still go out with my wife and my kids and coach them all the time. I think it’s just doing the things that I enjoy. Being a professional doesn't mean you need to ignore certain aspects of your life. I spent a lot of a lot of time learning that saying no doesn't mean you don't have to be you, it just means that you're focused on what you're trying to gain. I was focused on gaining my medical degree, my fellowship and ultimately my career. I'm just not going to let go of being me.
AM: As we get closer to the end of the year, are there any projects that you'd like to share that we should know about?
DR. CJR: In addition to my partnership with Sanofi and Regeneron on LungZone, another major project I am working on is developing a television program in which we educate people in a barber shop setting. There's a lot of education that happens at the barber shops. You know, I always have a dry erase pen with me so I can draw the science to help people understand, and I think taking that to a broader audience is extremely important. Being able to educate in any setting gives people the power to understand, and exposure to others who made them think about something in a different way. We have some prominent Hollywood producers and musicians involved and I think it’s going to a really positive platform that allows people to ask questions and find answers in an easy-to-understand way.
IG @DrJRutland
PHOTOS COURTESY | LungZone